Home » For Patients » Risk Factors
We don’t know what causes many NETs. Most seem to develop sporadically. Even though the causes of NETs are not largely known, we do know that some risk factors for neuroendocrine cancers can be passed down in families.
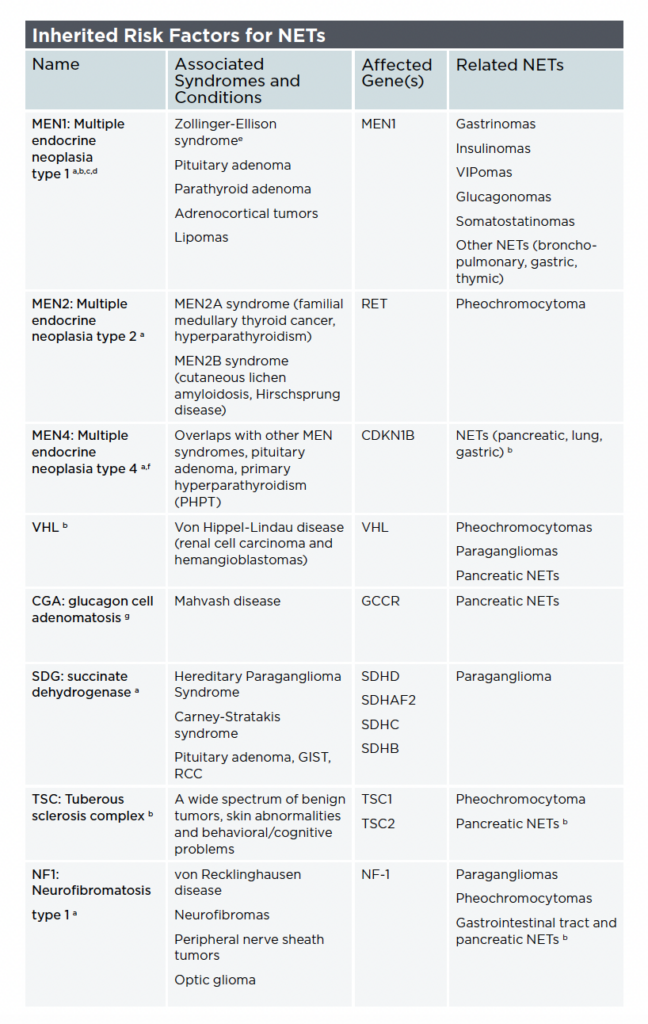
Researchers estimate that inherited factors may be associated with 10% of PNETs and 35% of pheochromocytomas and paragangliomas. Other rates vary depending on the primary site and subtypes of tumors.
Your medical history and your family’s medical history are part of the evaluation process. Having a first-degree relative with a known mutation also plays a vital role in establishing a clinical diagnosis. In some cases, the presence of two or more associated medical conditions or syndromes may indicate an inherited genetic condition.
Being aware that you have an inherited genetic risk factor will not always have an impact on your treatment plan but it may affect how your doctor monitors your health. If a genetic mutation is confirmed, your doctor may order additional testing regularly to look for other problems associated with that risk factor.
There are many different types of gene tests, which use a range of technologies. The gene testing kits advertised on TV (also known as direct-to-consumer testing) will probably not identify risk factors for NETs. Your doctor can order a test to look for specific mutations.
Your doctor may order genetic testing if your medical or family history indicates that you may have an inherited risk factor. Doctors can test for inherited mutations using blood or saliva.
Genetic testing looks for specific genes as well as certain changes in those genes. It is essential that your care team guides any decisions about genetic testing so the test results are reliable, accurate, and meaningful.
Genetic testing may not always be appropriate, especially if the results will not affect treatment planning. Genetic counseling can help you consider the risks, benefits, and limitations of genetic testing.
Genetic counseling includes a detailed review of an individual’s personal and family medical history that is relevant to the possible cancer of risk. Counseling also includes discussions about issues like:
Genetic tests may not be covered by all the insurance plans or may be covered only based on strict criteria. Contact your health insurance plan to learn more about your coverage and inquire about the costs before making any decisions about genetic testing.
Ask your doctor if there’s a genetic counselor who works with their team or look for a genetic counselor here.
There is little research to show potential connections between neuroendocrine neoplasms (NENs) such as NETs and environmental factors like chemical or other pollutant exposures. More research is needed to determine whether environmental exposures contribute to the formation of NETs and whether the impact of these exposures on any genetic predispositions may influence tumor development.
One study from 2002 identified certain occupational hazards as potential risk factors for NETs. Occupations like shoemaking, structural metal preparation, and construction painting that involve regular exposure to harmful substances like organic solvents and lead-containing paints may increase the risk for NETs. These associations could be coincidental rather than causative, and underscore the need for further research to fully understand their implications for NET development.
Another study from 2020 looked at early life exposures and associations with small-intestinal NETs. The researchers found an elevated risk for these NETs in those who may have been exposed in early life to industries such as the construction industry, uranium mining, and coal mining.
While most NENs are thought to arise sporadically, research has shown that a family history of cancer is a risk factor for NENs. Moreover, genetic syndromes such as von Hippel-Lindau disease and multiple endocrine neoplasia type 1 (MEN1) have an increased risk of NETs. These associations highlight the need for genetic screening and awareness in at-risk populations.
Identifying the risk factors in rare cancers poses significant challenges because it’s difficult to gather large, well-documented groups of people to study. Additionally, the field is hindered by a lack of adequate funding to study the epidemiology of NENs. These obstacles must be addressed to advance our understanding of NENs and their risk factors to ultimately improve patient outcomes.
NETs Risk Factors, by Lauren Fishbein, MD, PhD
Read about other NET patients and their journeys here.